Researchers Grow Humanized Mesonephros Inside Pig Embryos for 28 Days
On September 7th, LAI Liangxue’s group, PAN Guangjin’s group and Miguel A. Esteban’s group from Guangzhou Institutes of Biomedicine and Health (GIBH) of Chinese Academy of Sciences (CAS) published a cover paper together in the world's leading journal Cell Stem Cell. This paper reported generation of a humanized mesonephros in pigs from induced pluripotent stem cells via embryo complementation.
In this study, researchers created a novel human induced pluripotent stem cells (hiPSCs) with unrestricted lineage potential, enhanced competitiveness, and anti-apoptotic capability. Utilizing an optimized embryonic complementation technique, they successfully grow embryonic human kidneys inside nephric-deficient pigs for 28 days. This is the first time that scientists have been able to grow a solid human organ inside another species.
The shortage of donor organs represents the most challenging global problem. According to incomplete statistics, about 300,000 people with end-stage organ failure in China need transplants each year, but there are only around 20,000 operations because of shortages of organs. A promising alternative is to generate viable interspecies chimeras involving large mammals bearing human organs through embryo complementation with hiPSCs. The humanized organs generated by this strategy not only possess a comprehensive range of cell types, well-formed histological structure and functions, but also holds great potential to evade immune rejection due to their patient origin.
Integrating human stem cells into pig embryos faces many challenges, including poor differentiation potential and survival of hiPSCs in the xenogeneic embryos, lack of organogenesis-disabled niche in big animal hosts, as well as imperfect of embryonic complementation technique. PAN’s group has been working on mechanism of interspecies chimerism for years, and indicated that overexpressing the proliferation-promoting gene MYCN and the anti-apoptotic gene BCL2 effectively enhances the competitiveness and survival ability of hiPSCs inside xenogeneic embryos. Besides, a novel stem cell culture system developed by Esteban’s group, which efficiently generates human early embryonic-like stem cells with high chimeric capacity. LAI’s group combined multiplex-genes modification with somatic cell nuclear transfer, and created a novel pig model with nephric-defects. They successfully knocked out SIX1 and SALL1, which are essential for mesonephric tubule formation and ureteric bud invasion respectively, and generated a novel pig model with partial mesonephric-deficient and complete metanephros deficiency. LAI’s group also optimized the human-pig embryo complementation technique, which consist in the administration of three to five hiPSCs into morula or early blastocyst-stage pig embryos followed by culture in a medium composed of porcine zygote medium (PZM) and 4CL medium in a 1:1 ratio.
With the joint efforts of the three teams, they successfully grow embryonic human kidneys inside nephric-deficient pigs for 28 days. This study was performed in accordance with ethical rules and relevant international guidelines. The gestation of sows was terminated within 3-4 weeks. Overall, they obtained two embryos at 25 days and three embryos at 28 days. The proportion of human cells in the chimeric mesonephros reached up to 70%, and the proportion of human cell contribution in the formation of mesonephric tubules reached a maximum of 58%. Immunofluorescence staining of functional markers for kidney development, such as SIX1, SALL1, PAX2, and WT1, indicated that human donor cells could differentiate into functional cells. These results suggested that human donor cells could support the development of humanized kidneys in nephric-deficient pig embryos.
This study demonstrates proof-of-principle of the possibility of generating a humanized primordial organ in organogenesis-disabled pigs, opening an exciting avenue for regenerative medicine and an artificial window for studying human kidney development. It offers an attractive alternative to overcome the shortage of human organs for transplantation.
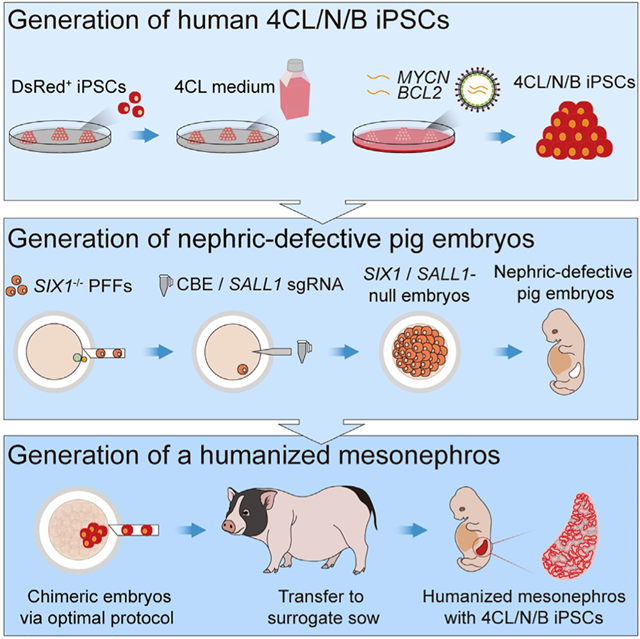
Fig.1 Graphical abstract of this study